Hip arthritis is a degenerative condition that affects the hip joint, and often leads to a significant impairment in the quality of life. The ability to walk, work and live pain free can be adversely affected. Approximately 43 million Americans suffer from arthritis and many of them are affected in the hip joint. In general, the treatment of hip arthritis involves activity modification, exercises, and treatment with anti-inflammatory medications. The use of assist devices such as canes, crutches or walkers can also be helpful. Occasionally surgical reconstruction such as total hip replacement is necessary.
Overview
What is the hip joint and what does it do?
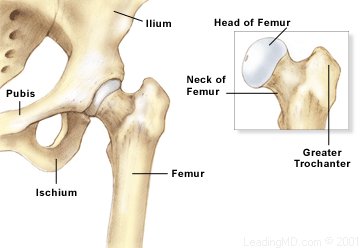
The hip joint is a ball and socket joint. The acetabulum, or socket, is formed by three areas of the pelvic structure: the ilium, the ischium, and the pubis. The femoral head is the "ball", which is located on the upper end of the femur. There is a high degree of fit and stability within this ball and socket joint. It is stabilized by strong ligaments in the front of the hip which prevent dislocation. Both the femoral head and the acetabulum are covered with a layer of cartilage which provides shock absorption and load distribution within the hip. This cartilage is also a source of nutrition for the joint. Numerous muscles play an important role in the stability of the hip, one of which is the gluteus medius. This is a deep muscle within the buttock, and its proper function is important in normal walking.
Function
Approximately 3 times the body weight is distributed through the hip with routine activities due to the muscle pull and joint forces that occur. Any degenerative condition within the hip will alter biomechanical relationships and can cause limping, leg length inequality and disability. The stability of the hip joint is maintained by the precise fit of the femoral head within the acetabulum. The hip allows rotation in many planes. These include: flexion/extension (used most commonly in sitting), internal and external rotation (used with twisting activities), and abduction and adduction (inward and outward motion of the hip in a scissoring action).
What is hip arthritis?
Hip arthritis is any condition that leads to degeneration of the hip joint and its cartilage surfaces. Some of these conditions are osteoarthritis, rheumatoid arthritis, avascular necrosis and congenital dysplasia (dislocation) of the hip. Fractures and other injuries to the hip joint can also lead to hip degeneration.
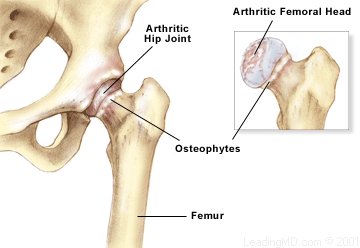
Osteoarthritis is a degenerative condition that may affect many joints throughout the body. It causes changes in the mechanical structure of the cartilage, which lead to its breakdown. Over time complete loss of the articular cartilage can occur. Changes in the underlying bone and loss of cartilage can result in joint space narrowing, peripheral osteophytes (bone spurs), loss of motion, pain and disability.
Rheumatoid arthritis is an inflammatory condition that affects the lining of all joints in the body. It causes an inflammatory response in the joint lining which destroys the articular cartilage and surrounding tissues.
Osteonecrosis or avascular necrosis is a condition in which the bone within the femoral head dies. This eventually leads to the collapse of large segments of the bone supporting the cartilage of the hip joint. It ultimately causes the destruction of the hip. The main causes of osteonecrosis include:
- injury such as femoral head fracture or hip dislocation.
- high dose corticosteroid employed in the treatment of lupus , asthma, and spinal cord injury.
- heavy alcohol abuse.
The final common pathway of hip arthritis is loss of the fit between the femoral head and the acetabulum. This results in thinning or complete loss of the cartilage, limitation of joint motion, shortening of the leg and continual pain and disability.
What are the symptoms of hip arthritis?
Most commonly, hip arthritis pain is described as increasing pain in the groin and anterior (front) thigh area. This usually begins with pain only during activities. It progresses to pain at rest and eventually disturbs sleep at night. With longstanding arthritis in the hip, motion in this area can be extremely limited, especially in flexion (bending) and internal rotation. Frequently, one limb becomes shorter than the other. Simple activities such as tying shoes and cutting toenails become compromised with advanced arthritis. A pronounced limp known as a Trendelenburg gait can result in which the shoulders move towards the side of the affected hip during weight bearing.
How is Hip Arthritis Diagnosed?
Hip arthritis can be diagnosed with a history of progressively increasing pain, first occurring with activities and eventually occurring at rest. Loss of motion in the hip also may be an indication of hip arthritis. Progressive limp and limb length inequality may be present as well. Hip arthritis should be clearly differentiated from other conditions that result in increasing pain such as hernias, aneurysms, and urologic and gynecologic problems.
Physical examination
The physician will check:
- The patient's gait to determine limb length inequality and the presence of Trendelenburg gait.
- Limb length assessment both in the standing and supine (prone) position may reveal that one leg is shorter than the other due to hip arthritis.
- Range of motion of the hip that shows a loss of internal rotation is a common sign of hip arthritis.
Difficulty in lifting the leg to the side may be present in severe cases. The hallmark of hip arthritis is pain with hip flexion and internal and external rotation. Another common symptom of hip arthritis is pain in the groin and on the outside thigh.
It is important to examine the lumbar spine for signs of herniated discs or radioulopathy since these conditions have symptoms similar to those of hip arthritis. Weakness in the leg, loss of sensation, reflex uneveness, pain with lumbar motion, or tenderness over the sacroiliac joint may all be signs that the hip complaints come from a condition in the back.
Diagnostic tests
Routine X-rays showing a standing front and rear view of the pelvis, and a "frogleg" lateral view will reveal arthritis signs such as:
- narrowing of the joint space.
- flattening of the subchondral (beneath the cartilage) bone.
- bone spur formation.
- limb length inequality.
Occasionally, oblique views of the pelvis are necessary to determine subtle dysplasia (abnormal tilt in the acetabulum) or abnormal formation of the acetabulum. MRI scanning and bone scanning may be used to detect other conditions such as the early stages of osteonecrosis of the femoral head.
How is hip arthritis treated?
The treatment of hip arthritis depends entirely upon severity of the patient's symptoms.
Non-Operative Treatment of Hip Arthritis
Early conditions are usually treated with:
- anti-inflammatory medications.
- exercise.
- weight loss.
- the use of walking aids.
- over the counter supplements for the building blocks of the articular cartilage.
People who have failed to improve with these non-operative measures may be candidates for surgical reconstruction. Most often, this is total hip replacement surgery. Patients who have severe pain with activities, pain at night, loss of the ability to work and perform routine activities, are those who may benefit from surgical treatment.
Surgical Treatment of Hip Arthritis
Total hip replacement surgery is very successful and has excellent short and long term outcomes. The surgeon removes the arthritis from the hip and inserts a metal and plastic prosthesis into the hip. This provides for hip function, limb length equality and restoration of motion. The procedure can be done with cement, which is a grout type of substance. It penetrates into the bone in both the acetabulum and the femur, providing fixation of the prosthesis to the bone. An alternative method uses uncemented components with roughened surfaces to which the bone adheres. (The bone grows into the rough titanium surface of the prosthesis). Both of these techniques have proven effective in long-term follow-up. The hospital stay lasts from 3-7 days following hip replacement surgery. The pain relief from removal of the hip arthritis is usually notable within the first week or two. After 3-6 months, most patients have recovered and returned to their normal lifestyles. Recovery includes physical therapy to regain strength and function, and often the use of a walker, crutches, or a cane for 4-8 weeks.
Complications
The complications from total hip replacement are infrequent but may be severe. These include (in the short term):
- infection at the rate of approximately 1%.
- dislocation: the femoral head prosthesis becomes dislodged from the socket. This often requires a procedure known as a closed reduction. In this operation the prosthesis is replaced in the socket under anesthesia.
- bleeding, requiring a blood transfusion.
- nerve injury.
- In some cases, the limb lengths cannot be made totally equal, and these patients may require a shoe-lift. This is most commonly seen in revision cases in which an existing hip prosthesis is removed and a second or third prosthesis is inserted over time.
Long term Complications
The most common reason for loosening of the components (they become dislodged from the bone) is long-term wear of the polyethylene liner, which leads to resorption (disappearance) of the bone layer next to the components. This occurs in both cemented and uncemented protheses. If the components become loose and the patient has symptoms, revision surgery may be an option. This involves removal of the existing prosthesis, followed by the insertion of new components and subsequent rehabilitation. The recovery from revision surgery is longer and more extensive than primary hip replacement surgery.
Overall, the complication rate from first hip replacement surgery is less than 5%. The long-term outcome of most conventional hip designs is roughly 80-85% survival at 15 years. Increased activity, improper lifting and improper precaution with the hip replacement may lead to early loosening and the need for revision. Fractures around the prosthesis both in the pelvis and in the femur may occasionally occur and may require surgical fixation.
Non-operative recovery:
Conservative measures, as described above, are used until they no longer provide adequate pain relief, and the functions of daily living become severely limited. Non-operative treatment usually results in some improvement in pain, endurance, and function. Very often non-operative treatment can not be indefinite.
Operative recovery:
Since arthritis or degenerative conditions within the hip are usually progressive, hip replacement surgery is often the choice when non-operative treatments no longer work.
Initial care of the hip replacement incision includes keeping it clean and dry for 7-14 days, followed by suture or staple removal. Certain precautions should be taken to prevent dislocation during the first 8 weeks. These are:
- No excessive flexion of the hip (such as being seated on a low toilet or on low chairs).
- Great care must be taken in rising from a prone to a standing position.
- and Great care must be taken getting in or out of a car.
- Patients should also be careful to not cross their legs, which may lead to dislocation.
- Aggressive activities such as heavy lifting or significant stair climbing must be avoided.
An exercise program is usually recommended for general conditioning of the leg during the rehabilitation process. Most patients, including those with non-cemented implants, are placed on protective weight-bearing with either crutches or a walker for 6-8 weeks following hip replacement surgery. The total recovery time, including return of muscle function, normalization of gait and improvement in quality of life may take 6-9 months. The pain relief from hip replacement surgery is usually immediate and long-lasting.
Follow-up
The fact that hip replacement components are artificial makes it especially important for the patient to return to the physician office for follow-up on a regular basis. Most physicians recommend annual follow up to assess the condition of the prosthesis, and evaluate the bone for underlying wear. An X-ray and physical examination will usually reveal any problems. Follow-up visits can help prevent devastating complications from loosening, wear, or fracture around the prosthesis.
Am I too young for hip replacement?
Older age is not a strict criterion for hip replacement. Incapacitating pain, limited function, and poor quality of life due to degeneration of the joint are the indications for hip replacement.
What are the most common complications from hip replacement?
Dislocation of the artificial joint is the most frequent complication of THR. Relocation of the joint usually requires anesthesia and may need brace or cast treatment after the joint is reduced. Infection, limb length, inequality, and bleeding are other less frequent complications.
How long do hip replacements last?
Modern hip replacements have a 90-95% survival rate at 15 years.