Orthopedic Shoulder Surgery and Replacement
Common Shoulder Injuries
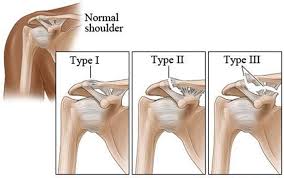
AC Separation
- Grade I - slight displacement of the joint. The acromioclavicular ligament may be stretched or partially torn. This is the most common type of injury to the AC joint.
- Grade II - partial dislocation of the joint in which there may be some displacement that may not be obvious during a physical examination. The acromioclavicular ligament is completely torn, while the coracoclavicular ligaments remain intact.
- Grade III - complete separation of the joint. The acromioclavicular ligament, the coracoclavicular ligaments, and the capsule surrounding the joint are torn. Usually, the displacement is obvious on clinical exam. Without any ligament support, the shoulder falls under the weight of the arm and the clavicle is pushed up, causing a bump on the shoulder.
- Grades IV through VI are rare, typically an injury from a car accident, and surgery is required for these.
Frozen Shoulder
- Freezing stage - pain is experienced when the shoulder has any sort of movement and your range of motion begins to decrease
- Frozen stage - the pain begins to decrease although the shoulder becomes more stiff, resulting in difficulty of performing daily activities
- Thawing stage - the pain continues to decrease and your range of motion begins to slowly increase until you have close to the normal range of motion
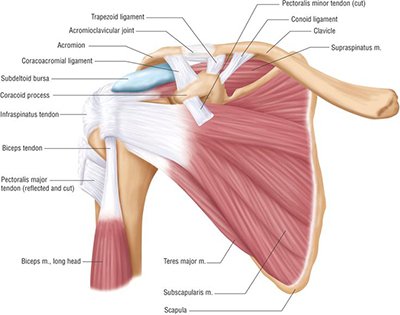
Rotator Cuff Tear
 classified as impingement syndrome or rotator cuff tears. Shoulder impingement syndrome occurs when the tendons of the rotator cuff are compressed as the shoulder is moving. This results in damage to the tendons and the bursa, a sac on top of your shoulder that allows the tendons to move freely, and pain is experience when the arm is raised away from the body. Impingement can develop over time with repetitive motions or as a result of an injury. There are three categories of impingement:
classified as impingement syndrome or rotator cuff tears. Shoulder impingement syndrome occurs when the tendons of the rotator cuff are compressed as the shoulder is moving. This results in damage to the tendons and the bursa, a sac on top of your shoulder that allows the tendons to move freely, and pain is experience when the arm is raised away from the body. Impingement can develop over time with repetitive motions or as a result of an injury. There are three categories of impingement:- Grade I - marked by inflammation of the bursa and tendons
- Grade II - progressive thickening and scarring of the bursa
- Grade III - rotator cuff degeneration and tears are evident
Shoulder Dislocation
Shoulder Labral Tears
Glenohumeral (Shoulder) Arthritis
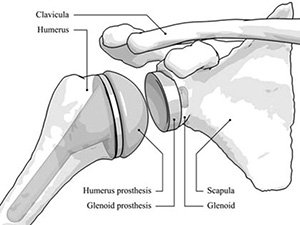
Total Shoulder Replacement
Making an Appointment
- Dr. Tom Hackett: Complex Knee, Shoulder & Elbow Surgeon
- Dr. Peter J. Millett: Shoulder, Knee, Elbow Surgery & Sports Medicine
- Dr. Matthew T. Provencher: Complex Shoulder, Complex Knee & Sports Surgery
- Dr. Armando F. Vidal: Complex Knee, Shoulder & Sports Medicine Surgeon
- Dr. Leslie B. Vidal: Shoulder, Hip, Knee & Sports Medicine Specialist
- Dr. Jonathan A. Godin: Shoulder, Knee, Hip & Sports Medicine Surgeon
- Dr. Jared T. Lee: Shoulder, Hip, Knee & Sports Medicine
- Dr. Joseph J. Ruzbarsky: Shoulder, Knee, Elbow & Hip Preservation Surgery
- Driver’s License or a valid ID
- List of Medications
- Insurance Information
- Any other relevant medical information
When preparing for your shoulder procedure it is important to think through what will be needed post surgery. For example what changes will need to be made at home and how much time should you take off work. Be sure to make a list of any questions that you may have to ask your shoulder surgeon prior to surgery.
It can also be helpful to meet with your physical therapist prior to your surgery as doing some of the postoperative exercises before can help with recovery. It you are overweight, it is recommended that you try to lose a few pounds prior to surgery as that will also help with recovery.
For more on how to prepare for your shoulder surgery, please visit our Preparing for Surgery page.
Depending on the severity of the injury, the recovery process following shoulder surgery can be up to 4 to 6 months.
Following your surgery you will typically begin a customized physical therapy plan developed specifically for you and your shoulder injury. The physical therapist (PT) will go over specific exercises that will help you to reduce stiffness and regain full shoulder movement
The length of your hospital stay will also depend on your surgery and the recommendation of your doctor. Once you are released to go home, you will continue physical therapy for the designated period your doctor has prescribed.
Read more on Rehabilitation and Training.
- Frozen Shoulder
- Rotator Cuff / Impingement
- AC Separation
- Shoulder Instability
- Multidirectional Instability
- Labral Tears
- Glenohumeral (Shoulder) Arthritis
- Total Shoulder Replacement